If you understand math, the answer may be quite simple when you look at the numbers. If you don’t particularly enjoy or understand math, here is a primer. Polyamorous relationships and open marriages expose individuals to higher risks of sexually transmitted infections (STIs) and sexually transmitted diseases (STDs) compared to monogamous relationships. However, the risk depends heavily on sexual behavior, partner selection, and safe sex practices. Here’s an outline of the factors involved in the risk of exposure:
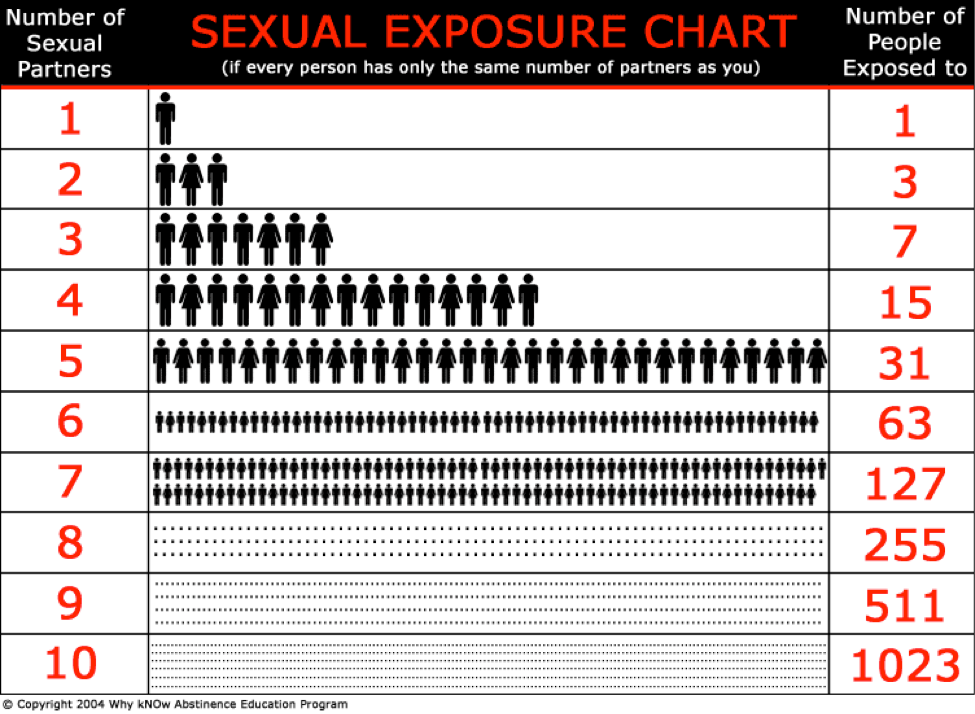
- Number of Sexual Partners: The primary factor for increased risk of STIs is the number of sexual partners. Research indicates that a higher number of partners leads to greater exposure, as each partner brings their sexual network into the relationship. For instance, individuals who reported multiple partners had a significantly higher risk of contracting STIs like chlamydia and gonorrhea (SpringerLink)(BioMed Central). The risk amplifies with each additional partner, especially when considering the sexual behavior of those partners and their previous sexual encounters (BioMed Central).
- Partner’s Sexual Network: The sexual history of partners plays a crucial role in STI transmission. In polyamorous relationships, even if one partner is practicing safe sex, their other partners may not be, increasing the risk for everyone involved. Individuals often underestimate the number of their partner’s sexual encounters, which further complicates risk assessments (BioMed Central).
- Frequency of Sexual Encounters: The more frequently sexual encounters occur, especially with different partners, the higher the probability of STI transmission. This frequency, paired with a lack of condom use, significantly elevates risk (SpringerLink).
According to the CDC, about 12% of sexually active women aged 15–44 have been tested for STIs (excluding HIV) in the last year, while the percentage is lower for men. — CDC
Increased Risk Relative to Monogamy:
Polyamorous individuals are often more conscientious about sexual health than those in traditional monogamous relationships. Studies suggest that people in polyamorous communities may engage in more frequent STI testing and use protection, particularly condoms, more consistently (Dr. Liz Powell). Despite this, the simple math of more sexual partners creates additional risk vectors, even with precautions.
Dormancy and Detection of STIs:
- Chlamydia and Gonorrhea: Symptoms can take anywhere from 1 to 3 weeks to appear, but both can also remain asymptomatic for longer, which is why frequent testing is critical.
- Herpes (HSV-1 and HSV-2): The virus can remain dormant for months or even years, with outbreaks triggered by stress or illness.
- HIV: It may take several weeks to months for symptoms to appear, and HIV can be undetectable during this window, further increasing the risk when partners are not regularly tested (Dr. Liz Powell).
Fewer than 40% of adults aged 18–44 report ever being tested for an STI outside of routine Pap smears and other standard exams. — CDC
Prevention and Risk Mitigation:
- Regular Testing: Those in polyamorous and open relationships often undergo frequent STI testing, sometimes more rigorously than individuals in monogamous relationships, as open communication about sexual health is vital (Dr. Liz Powell).
- Barrier Methods: Consistent use of condoms and dental dams significantly reduces the risk of STI transmission, particularly for bacterial infections like gonorrhea and syphilis.
- Open Communication: Ensuring that all partners are informed about sexual history, testing results, and any STIs is critical. Experts emphasize that open communication in polyamorous relationships often leads to better sexual health outcomes than in some monogamous relationships, where such discussions may be stigmatized (Dr. Liz Powell).
In summary, practicing polyamory and open marriage increases the potential for STI transmission due to the larger sexual network. While practicing regular testing, using protection, and maintaining transparent communication about sexual health can help mitigate these risks, there are many fail points in the process.
The rate at which sexually active individuals test for STDs and STIs varies widely, but research shows that testing remains relatively low despite increasing awareness. According to the CDC, about 12% of sexually active women aged 15–44 have been tested for STIs (excluding HIV) in the last year, while the percentage is lower for men. Overall, fewer than 40% of adults aged 18–44 report ever being tested for an STI outside of routine Pap smears and other standard exams.
Testing frequencies also depend on sexual behaviors and demographics. For instance, men who have sex with men (MSM) are encouraged to test more frequently, at least annually, or even more often depending on their risk factors. MSM and other high-risk populations like those with multiple partners or inconsistent condom use are strongly advised to test every 3–6 months. However, studies show that 53% of STIs in the U.S. occur among young people aged 15–24, a group that often does not test regularly (CDC)(Verywell Health).
The COVID-19 pandemic negatively impacted testing rates, reducing overall screenings and leaving many individuals undiagnosed. For example, cases of chlamydia dropped during the pandemic, not necessarily because of fewer infections, but likely because fewer people were getting tested (Verywell Health).
This data suggests that even though awareness of STIs is rising, regular testing remains uncommon among sexually active individuals, especially those who don’t perceive themselves as high-risk. Health organizations recommend routine testing as a preventive measure to manage the rising rates of STIs.
Safe Sex?
In conclusion, the premise that safe sex is truly safe is inconsistent with real-world behaviors and biological realities. The low rates of STD and STI testing, the improper and inconsistent use of contraceptives, and the increasing prevalence of non-monogamous sexual practices all contribute to a heightened risk of infection. Additionally, the dormancy and asymptomatic nature of many STDs and STIs mean that even those who believe they are practicing safe sex can unwittingly spread infections to others.
While condoms and other protective measures are effective at reducing risk, they do not eliminate it. The belief that safe sex is a foolproof strategy is a dangerous misconception. As sexual behaviors continue to evolve and the number of sexual partners increases, so too does the complexity and risk of sexually transmitted infections. The key takeaway is that safe sex is not risk-free, and relying solely on protective measures without regular testing and communication with partners is not a guarantee of safety.
Recovering From Infidelity
If you have experienced infidelity-induced trauma caused by the emotional and sexual betrayal of your spouse, there is hope! If you are a child affected by parental infidelity, there is hope! If you are a spouse who has betrayed your marriage’s trust, love, and fidelity, there is hope! We recommend that you seek support through professional counseling and therapy as well as through groups dedicated to supporting you through this traumatic journey. You are not alone and recovery and healing are possible!
Share Your Story
The CHADIE Foundation shares personal stories of spouses and children impacted by infidelity and affairs. If you have a story you want to share and have published, please use the contact information below to share your story with The CHADIE Foundation. Our mission is to help educate everyone about the damage infidelity, affairs, and adultery cause families and how to minimize the impact.
About CHADIE Foundation
The CHADIE Foundation (Children are Harmed by Adultery, Divorce, Infidelity, and related Emotional trauma), helps spouses, partners, and children who adultery, affairs, and infidelity have negatively impacted. To learn more about CHADIE and how you can help, please email us at support@chadie.org or visit us at CHADIE.org.